Now Reading: Understanding the Luteal Phase: A Complete Guide
-
01
Understanding the Luteal Phase: A Complete Guide
Understanding the Luteal Phase: A Complete Guide
The menstrual cycle is more than just your period; it’s a complex and fascinating process that prepares your body for a potential pregnancy each month. It’s composed of different stages, each with its unique hormonal shifts and physical changes. One of the most significant of these is the luteal phase. This stage occurs after ovulation and plays a crucial role in fertility and your overall menstrual health.
Understanding the luteal phase can empower you to better interpret your body’s signals, manage symptoms like PMS, and gain insights into your reproductive health. Whether you’re trying to conceive, tracking your cycle for wellness, or are simply curious about how your body works, this guide will walk you through everything you need to know about this important time.
Key Takeaways
- The luteal phase is the second half of your menstrual cycle, beginning after ovulation and ending when your period starts.
- It typically lasts between 12 to 14 days and is dominated by the hormone progesterone.
- Progesterone’s main job during this phase is to thicken the uterine lining (endometrium) to support a potential pregnancy.
- Common symptoms include breast tenderness, bloating, mood changes, and food cravings, often associated with Premenstrual Syndrome (PMS).
- A short luteal phase (less than 10 days) may indicate low progesterone and can make it harder to sustain a pregnancy.
What Exactly Is the Luteal Phase?
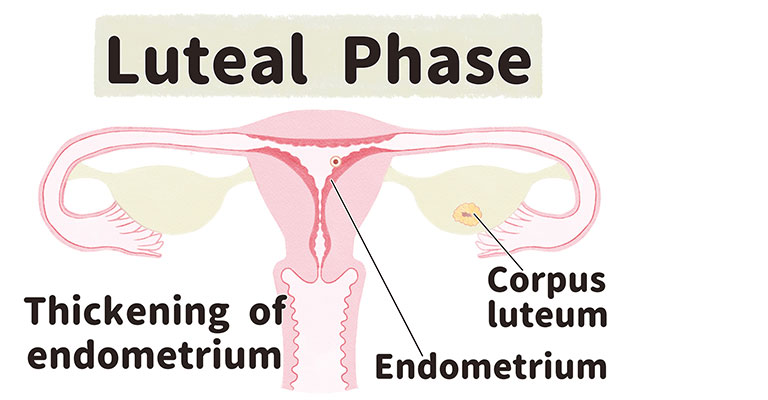
The luteal phase is the final stage of the menstrual cycle. It starts on the day after ovulation and continues until your next period begins. This phase is named after the corpus luteum, a temporary structure that forms in the ovary from the follicle that released an egg during ovulation. Think of the corpus luteum as a tiny, temporary hormone factory. Its primary job is to produce progesterone, the star hormone of the luteal phase.
Progesterone signals the lining of your uterus, called the endometrium, to thicken and mature. This creates a nourishing and stable environment for a fertilized egg to implant and grow. If pregnancy doesn’t occur, the corpus luteum breaks down, progesterone levels fall, and the uterine lining is shed, starting your menstrual period. This entire process is a brilliant example of your body’s intricate hormonal orchestra working in harmony.
The Two Halves of the Menstrual Cycle
To fully grasp the luteal phase, it helps to see where it fits into the bigger picture. The menstrual cycle is generally divided into two main parts:
- The Follicular Phase: This is the first half. It starts on day one of your period and ends with ovulation. During this time, the hormone estrogen rises, stimulating follicles in your ovaries to mature an egg.
- The Luteal Phase: This is the second half. It begins right after the egg is released (ovulation) and ends with the start of your next period. This phase is characterized by high levels of progesterone.
Understanding these two halves helps you see the cycle as a continuous loop, with each phase setting the stage for the next.
How Long Does the Luteal Phase Last?
For most individuals, a healthy luteal phase lasts between 12 and 14 days. While the length of the follicular phase can vary significantly from person to person (and even from cycle to cycle), the luteal phase is generally more consistent. Its stability is one of the key indicators of regular ovulation and sufficient progesterone production.
A phase that is consistently shorter or longer than this average range might be worth discussing with a healthcare provider. A short luteal phase, in particular, can be a concern for those trying to conceive, as it may not give a fertilized egg enough time to implant securely in the uterine wall. Tracking your cycle can give you valuable data on the length and consistency of your personal luteal phase.
What Is a Short Luteal Phase?
A luteal phase that lasts for 10 days or less is considered short. This condition, sometimes called a luteal phase defect, means the body may not be producing enough progesterone to fully prepare the uterine lining for pregnancy. As a result, even if an egg is fertilized, it may struggle to implant, or the lining may begin to shed too early. This can lead to difficulty conceiving or early pregnancy loss. If you track your cycle and suspect you have a short luteal phase, consulting a doctor is a good next step. They can perform tests to check hormone levels and recommend potential treatments.
What About a Long Luteal Phase?
A luteal phase that extends beyond 16-18 days without a period starting could be a sign of one of two things:
- Early Pregnancy: The most common reason for a long luteal phase is pregnancy. When a fertilized egg implants, it begins to produce the hormone human chorionic gonadotropin (hCG). This is the hormone detected in pregnancy tests. hCG signals the corpus luteum to continue producing progesterone, which maintains the uterine lining and prevents your period from starting.
- Hormonal Imbalance: Less commonly, a long luteal phase without pregnancy could indicate a hormonal issue, such as a persistent ovarian cyst that continues to produce progesterone.
If your period is late and you’ve had a luteal phase longer than 18 days, it’s a good time to take a home pregnancy test.
Hormonal Changes During the Luteal Phase
Hormones are the chemical messengers that drive the entire menstrual cycle. During the luteal phase, the hormonal landscape shifts dramatically from the first half of your cycle.
- Progesterone: This is the dominant hormone. After ovulation, progesterone levels surge, thanks to the corpus luteum. Its mission is to make the uterus a welcoming home for a potential embryo. It causes the uterine lining to become thick, spongy, and rich with blood vessels. Progesterone also has a calming effect on the uterine muscle to prevent contractions that could interfere with implantation.
- Estrogen: While progesterone takes the lead, estrogen also remains present. It works alongside progesterone to help prepare the endometrium. However, its levels are much lower than during the follicular phase.
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH): The surge of LH is what triggers ovulation, marking the start of the luteal phase. After this peak, both LH and FSH levels drop and remain low throughout this stage.
If pregnancy does not occur, the corpus luteum begins to degrade about 10 to 12 days after ovulation. This causes both progesterone and estrogen levels to plummet, triggering the shedding of the uterine lining and the start of your period.
|
Hormone |
Role in the Luteal Phase |
|---|---|
|
Progesterone |
Dominant hormone; thickens the uterine lining for implantation. |
|
Estrogen |
Plays a supporting role in preparing the uterine lining. |
|
LH & FSH |
Levels remain low after triggering ovulation. |
|
hCG |
Appears only if pregnancy occurs; sustains progesterone production. |
Common Luteal Phase Symptoms
The significant hormonal fluctuations during the luteal phase can cause a wide range of physical and emotional symptoms. Many people are familiar with these as symptoms of Premenstrual Syndrome, or PMS. The rise in progesterone is primarily responsible for these changes.
Physical Symptoms
- Breast Tenderness: Progesterone can cause the milk ducts in your breasts to grow, leading to soreness, swelling, or a heavy feeling.
- Bloating and Water Retention: Progesterone can slow down your digestion, leading to gas and constipation. It also contributes to the body holding onto more water.
- Acne Breakouts: Hormonal shifts can increase oil production in your skin, potentially clogging pores and causing pimples.
- Headaches: For some, the drop in estrogen and progesterone right before the period starts can trigger hormonal headaches or migraines.
- Food Cravings: Fluctuating hormones and blood sugar levels can lead to cravings, often for salty, sweet, or carb-heavy foods.
- Fatigue: The rise in progesterone can have a slightly sedative effect, leaving you feeling more tired or sluggish than usual.
Emotional and Mood Symptoms
- Mood Swings: You might feel more irritable, anxious, or weepy during the luteal phase. This is a very common response to the hormonal shifts.
- Difficulty Concentrating: Some people report feeling “brain fog” or find it harder to focus on tasks.
- Changes in Libido: Libido often decreases during this time due to lower estrogen and testosterone levels compared to the ovulatory phase.
It’s important to remember that experiencing some of these symptoms is normal. However, if they are severe enough to disrupt your daily life, you may be dealing with Premenstrual Dysphoric Disorder (PMDD), a more severe form of PMS that warrants a discussion with a healthcare professional.
How to Track Your Luteal Phase
Tracking your luteal phase is a powerful way to understand your unique cycle. To know when your luteal phase begins, you first need to pinpoint the day of ovulation. There are several methods you can use, often in combination, for the most accurate results.
Basal Body Temperature (BBT) Charting
Your basal body temperature is your lowest resting body temperature. By taking your temperature with a special BBT thermometer first thing every morning, you can identify a sustained temperature shift. After ovulation, the rise in progesterone causes a slight but noticeable increase in your BBT (about 0.5 to 1.0°F), which remains elevated throughout the luteal phase. This temperature shift confirms that ovulation has already happened.
Ovulation Predictor Kits (OPKs)
These kits are urine tests that detect the surge in Luteinizing Hormone (LH) that occurs 24-36 hours before ovulation. A positive OPK tells you that ovulation is about to happen, allowing you to predict the start of your luteal phase.
Cervical Mucus Monitoring
The consistency of your cervical mucus changes throughout your cycle. Around ovulation, it becomes clear, slippery, and stretchy, resembling raw egg whites. After ovulation, as progesterone rises, it typically becomes thicker, stickier, or creamy, or it may dry up completely. Observing these changes can help you identify your fertile window and the shift into the luteal phase.
Once you’ve confirmed your ovulation day, you can count the days until your next period starts. That number is the length of your luteal phase. Doing this for a few cycles will give you a clear average.
Luteal Phase and Fertility
The luteal phase is absolutely critical for anyone trying to conceive. A healthy uterine lining is just as important as a healthy egg and sperm. For a successful pregnancy to begin, the endometrium must be “receptive”—thick, nourished, and ready for an embryo to attach. This is entirely dependent on adequate progesterone production during the luteal phase.
If the luteal phase is too short (a luteal phase defect), the uterine lining may not have enough time to develop properly. Even if fertilization occurs, the embryo may arrive in the uterus before the environment is ready for it, preventing implantation. This is a common and often treatable cause of infertility.
For those undergoing fertility treatments like IVF, the luteal phase is carefully managed. Doctors often prescribe progesterone supplements (in the form of pills, suppositories, or injections) to ensure the uterine lining is perfectly prepared and supported during the crucial early weeks of pregnancy. You can find more insights on related health topics at resources like forbesplanet.co.uk.
Supporting a Healthy Luteal Phase
While your hormones largely run the show, certain lifestyle habits can help support a balanced and healthy luteal phase.
Nutrition for Your Luteal Phase
- Focus on Nutrient-Dense Foods: Eat plenty of whole foods, including leafy greens, colorful vegetables, healthy fats, and quality proteins. These provide the building blocks your body needs to produce hormones.
- Incorporate B Vitamins: Vitamin B6, in particular, is thought to play a role in the development of the corpus luteum and the production of progesterone. You can find it in foods like chickpeas, tuna, salmon, potatoes, and bananas.
- Manage Blood Sugar: Progesterone can affect insulin sensitivity. Stabilize your blood sugar by eating balanced meals with protein, fat, and complex carbohydrates (like sweet potatoes and whole grains) to help manage mood swings and energy levels.
- Stay Hydrated: Drinking plenty of water can help alleviate bloating and constipation, which are common symptoms during this time.
Lifestyle and Stress Management
Stress is a major disruptor of hormonal balance. High levels of the stress hormone cortisol can interfere with the production of progesterone. Finding effective ways to manage stress is key to supporting a healthy luteal phase.
- Prioritize Sleep: Aim for 7-9 hours of quality sleep per night. Sleep is when your body repairs itself and regulates hormones.
- Gentle Movement: Intense exercise can be a form of stress on the body. During the luteal phase, consider shifting to more restorative activities like walking, yoga, swimming, or stretching.
- Practice Mindfulness: Activities like meditation, deep breathing exercises, or journaling can help calm your nervous system and reduce cortisol levels. Even just a few minutes a day can make a difference.
When to See a Doctor
While some fluctuations and symptoms are normal, certain signs may indicate it’s time to speak with a healthcare provider about your luteal phase.
Consider making an appointment if you experience:
- Consistently short cycles (24 days or less), which may point to a short luteal phase.
- Spotting for several days between ovulation and your period.
- Difficulty conceiving after a year of trying (or six months if you are over 35).
- Severe PMS or PMDD symptoms that interfere with your work, relationships, or daily life.
- Very irregular cycles, which can make it difficult to even identify your luteal phase.
A doctor can run blood tests to check your progesterone levels (typically done about seven days after ovulation) and other hormones to get a clear picture of what’s happening.
Frequently Asked Questions (FAQ)
Q: Can you get pregnant during the luteal phase?
A: Conception (fertilization) happens around ovulation, just before the luteal phase begins. The luteal phase is the period after ovulation where implantation occurs. Since the egg only survives for about 12-24 hours after being released, you cannot get pregnant from intercourse that takes place several days into your luteal phase. The fertile window closes about a day after ovulation.
Q: Does basal body temperature stay high during the luteal phase if you’re pregnant?
A: Yes. If you become pregnant, your BBT will remain elevated past the typical length of your luteal phase. An elevated temperature for 18 days or more after ovulation is a strong early indicator of pregnancy. If you are not pregnant, your temperature will drop just before or when your period starts.
Q: What is a luteal phase defect?
A: A luteal phase defect (LPD) is a condition where the uterine lining doesn’t develop properly due to insufficient progesterone production or the lining’s inability to respond to progesterone. This is often associated with a short luteal phase (10 days or less) and can make it difficult to achieve or maintain a pregnancy.
Q: Can stress make my luteal phase shorter?
A: Yes, significant physical or emotional stress can disrupt your hormonal balance. The stress hormone cortisol can suppress the hormones needed for healthy ovulation and progesterone production, which can potentially lead to a shorter luteal phase.
Q: Are PMS and luteal phase symptoms the same thing?
A: Essentially, yes. The symptoms commonly known as PMS (Premenstrual Syndrome) occur during the luteal phase. They are the body’s response to the hormonal shifts, particularly the rise and subsequent fall of progesterone, that characterize this stage of the cycle.
Conclusion
The luteal phase is a dynamic and vital part of your monthly cycle. Governed by progesterone, its primary purpose is to prepare your body for a potential pregnancy, but its influence extends to your mood, energy, and overall well-being. By learning to identify and track your luteal phase, you can gain incredible insight into your reproductive health.
Paying attention to its length and the symptoms you experience can help you advocate for yourself at the doctor’s office, make informed decisions about family planning, and implement lifestyle changes that support your hormonal health. Embracing this knowledge empowers you to work with your body’s natural rhythms, fostering a deeper connection to and appreciation for its incredible capabilities.