Now Reading: What Does Poop Look Like with Diverticulitis? A Complete Guide
-
01
What Does Poop Look Like with Diverticulitis? A Complete Guide
What Does Poop Look Like with Diverticulitis? A Complete Guide

Dealing with digestive issues can be confusing and a little scary. When your body starts sending you signals you don’t understand, like changes in your bowel movements, it’s natural to have questions. One common condition that affects the digestive tract is diverticulitis. Many people wonder about its symptoms, particularly how it affects their stool. Understanding these changes is a key part of managing your health and knowing when to seek medical advice.
This guide is here to provide clear, friendly information about diverticulitis and its impact on your bowel habits. We will explore what does poop look like with diverticulitis, break down the reasons for these changes, and discuss how diet and treatment can help. Our goal is to give you the knowledge you need to feel more confident and in control of your digestive health.
Key Takeaways
- Diverticulitis can cause significant changes in stool, including alterations in color, shape, and consistency.
- Common changes include thin, pellet-like stools, diarrhea, constipation, and sometimes mucus or blood.
- These changes are often due to inflammation, muscle spasms in the colon, and dietary adjustments during a flare-up.
- Observing your stool is an important way to monitor your condition, but it’s not a standalone diagnostic tool.
- A healthcare provider should always be consulted for an accurate diagnosis and a personalized treatment plan.
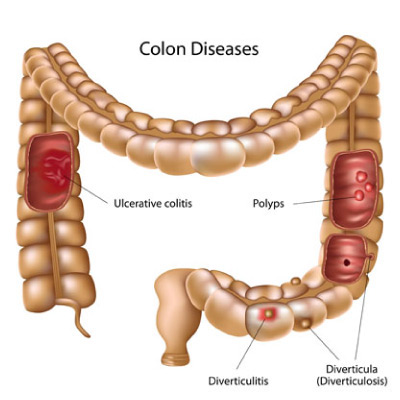
Understanding Diverticulitis and Diverticulosis
Before we dive into the specifics of bowel movements, it’s important to understand the difference between two related conditions: diverticulosis and diverticulitis. Though they sound similar, they are not the same thing.
Diverticulosis refers to the presence of small, bulging pouches (called diverticula) that can form in the lining of your digestive system. These pouches most often develop in the lower part of the large intestine, also known as the colon. Diverticula are quite common, especially as people age. It’s estimated that over half of people over the age of 60 have them. Most individuals with diverticulosis have no symptoms and may never even know they have it. It is often discovered during a routine colonoscopy or other medical test for an unrelated issue.
Diverticulitis, on the other hand, occurs when one or more of these pouches become inflamed or infected. This is when symptoms typically appear. The inflammation can cause a range of issues, from mild discomfort to severe pain, fever, and nausea. It is this inflammatory process that leads to noticeable changes in your body, including alterations in your bowel habits. While diverticulosis is the underlying condition, diverticulitis is the active, symptomatic phase that requires medical attention.
What Causes Diverticula to Form?
Researchers believe that diverticula form when naturally weak spots in the outer layer of the colon give way under pressure. This pressure can cause the inner layers to bulge outward, creating the small pouches. A leading theory suggests that a low-fiber diet plays a significant role. Without enough fiber to add bulk to the stool, the colon has to work harder to push smaller, harder stools through. This increased strain and pressure over many years may lead to the formation of diverticula. Other factors like genetics, lack of exercise, obesity, and smoking can also increase your risk.
What Does Poop Look Like with Diverticulitis? The Detailed Answer
When diverticulitis strikes, the inflammation and infection in your colon can have a direct impact on your stool. The appearance can vary from person to person and depends on the severity of the flare-up. Let’s break down the most common changes you might observe.
Changes in Stool Shape and Consistency
One of the most frequently reported changes during a diverticulitis flare-up is an alteration in the shape and consistency of your poop.
Thin, Ribbon-Like, or Pellet-Like Stools
During an active bout of diverticulitis, the colon can become very inflamed and swollen. This inflammation can narrow the inside of the intestine, acting like a partial blockage. As stool passes through this constricted area, it can be squeezed into a thinner, more narrow shape. This is why many people describe their poop as being thin, stringy, or ribbon-like.
Additionally, muscle spasms in the colon wall, triggered by the inflammation, can cause stool to break apart into small, hard pieces. This can result in pellet-like stools, similar to what is often seen with constipation. The combination of inflammation and spasms makes it difficult for the colon to form and pass a normal, well-formed stool. It’s important to note that persistent thin stools should always be evaluated by a doctor, as they can also be a sign of other conditions.
Diarrhea or Loose Stools
While some people experience constipation and hard stools, others may have the opposite problem: diarrhea. The inflammation from diverticulitis can irritate the lining of the colon, causing it to secrete more mucus and water. This irritation can also speed up the transit time of waste through the digestive system, leaving less time for water to be absorbed. The result is frequent, loose, and watery stools. Diarrhea can be particularly concerning because it can lead to dehydration and electrolyte imbalances, especially if it is severe or persistent.
Alternating Between Constipation and Diarrhea
For some individuals, diverticulitis can create a confusing cycle of alternating between constipation and diarrhea. You might have several days of difficulty passing small, hard stools, followed by a sudden bout of urgent, loose stools. This unpredictable pattern is a result of the colon’s erratic behavior as it struggles with inflammation, muscle spasms, and irritation. The digestive system is thrown off balance, leading to inconsistent bowel function that can be frustrating and uncomfortable to manage.
Color Changes in Stool with Diverticulitis
The color of your poop can also provide clues about what’s happening inside your digestive tract. While diet and medications can influence stool color, certain changes may be directly related to a diverticulitis flare-up.
Dark or Bright Red Stools (Blood)
The presence of blood is one of the more alarming symptoms you might notice. With diverticulitis, bleeding can occur, though it’s more common with a related condition called diverticular bleeding (where a blood vessel within a pouch ruptures).
- Bright Red Blood: This usually indicates that the bleeding is happening in the lower part of the colon or the rectum. The blood looks fresh because it hasn’t had time to be digested. You might see it on the toilet paper, in the toilet bowl water, or streaked on the surface of the stool.
- Dark Red or Maroon Stools: This suggests the bleeding is occurring higher up in the colon. The blood has had more time to mix with the stool and begin to break down, giving it a darker color.
Any amount of blood in your stool is a reason to contact your doctor immediately. While it can be a symptom of diverticulitis, it can also signal other serious conditions, and it’s crucial to get a proper diagnosis.
Dark, Tarry Stools
Very dark, black, or tarry-looking stools can also be a sign of bleeding, but it typically points to bleeding in the upper gastrointestinal tract, such as the stomach or small intestine. When blood is exposed to digestive enzymes for a longer period, it turns black and gives the stool a sticky, tar-like consistency. While less common with diverticulitis, which affects the lower GI tract, it’s not impossible if bleeding is slow and transit time is delayed. However, it’s important to rule out other causes, like taking iron supplements or certain medications like Pepto-Bismol, which can also turn stool black.
Mucus in the Stool
It’s normal for the colon to produce a small amount of mucus to help lubricate the passage of stool. However, during a diverticulitis flare-up, the inflammation can cause the colon to produce excess mucus. You might notice slimy, stringy, or jelly-like substances mixed in with your stool or coating it. While seeing some mucus can be normal, a significant increase is often a sign of irritation or inflammation in the intestines and is commonly reported by those with diverticulitis.
Why Does Diverticulitis Change Your Poop?
Understanding what does poop look like with diverticulitis is one part of the puzzle. The other is knowing why these changes happen. Several factors contribute to the altered appearance of your stool during a flare-up.
|
Cause |
Effect on Stool |
Explanation |
|---|---|---|
|
Inflammation and Swelling |
Thin, ribbon-like stools |
The inflamed intestinal wall narrows the colon, squeezing the stool as it passes through. |
|
Muscle Spasms |
Pellet-like stools, constipation, abdominal cramping |
Inflammation can cause the colon muscles to contract erratically, breaking up stool and making it harder to pass. |
|
Dietary Changes |
Hard stools or loose stools |
During a flare-up, doctors often recommend a clear liquid or low-fiber diet, which lacks the bulk needed to form normal stools. |
|
Infection and Irritation |
Diarrhea, mucus in stool |
An infection irritates the colon lining, leading to increased water and mucus secretion and faster transit time. |
|
Bleeding |
Red or dark-colored stools |
Inflammation can erode a blood vessel in a diverticulum, causing bleeding into the colon. |
The Role of a Low-Fiber Diet During a Flare-Up
When you’re experiencing a diverticulitis flare-up, your doctor will likely recommend a temporary change in your diet. The primary goal is to give your colon a chance to rest and heal. This usually means starting with a clear liquid diet for a few days. This includes things like water, broth, clear juices without pulp, and gelatin.
As you start to feel better, you’ll slowly transition to a low-fiber diet. This includes foods like white bread, white rice, pasta, and well-cooked vegetables without skins. While this diet is crucial for healing, it has a direct impact on your stool. Fiber is what gives stool its bulk and soft texture. Without it, your poop is likely to be smaller, harder, and more difficult to pass. This dietary change is a major reason why constipation and pellet-like stools are so common during and immediately after a diverticulitis flare-up. For more in-depth health insights, you can explore resources like those found at https://forbesplanet.co.uk/.
When to See a Doctor
Self-monitoring your symptoms is helpful, but it’s not a substitute for professional medical care. It is essential to see a doctor for a proper diagnosis and treatment plan. Contact your healthcare provider if you experience any of the following:
- Persistent abdominal pain, especially if it’s severe and localized (often on the lower left side).
- Fever and chills, which can indicate an infection.
- Nausea and vomiting, which prevent you from keeping fluids down.
- Any blood in your stool, whether it’s bright red, maroon, or black.
- A sudden and significant change in your bowel habits that doesn’t resolve.
- Inability to pass stool or gas, which could be a sign of a blockage.
A doctor can perform a physical exam and may order tests like a CT scan, blood tests, or a stool sample analysis to confirm a diagnosis of diverticulitis and rule out other conditions. Early diagnosis and treatment are key to preventing complications.
Potential Complications of Untreated Diverticulitis
Ignoring the symptoms of diverticulitis can lead to serious health problems. The inflammation and infection can worsen, leading to complications such as:
- Abscess: A painful, pus-filled pocket that forms outside the colon wall.
- Fistula: An abnormal connection or tunnel that forms between the colon and another organ, like the bladder or vagina.
- Perforation: A tear or hole in an inflamed pouch, which can spill intestinal contents into the abdominal cavity, causing a life-threatening infection called peritonitis.
- Bowel Obstruction: Severe inflammation or scarring can cause a partial or complete blockage of the colon.
These complications often require more intensive treatments, including hospitalization, intravenous antibiotics, or even surgery. This is why seeking prompt medical care is so important.
Managing Diverticulitis and Improving Bowel Health
Once a diverticulitis flare-up is under control, the focus shifts to long-term management and prevention. The goal is to keep your colon healthy and reduce the risk of future flare-ups.
The Importance of a High-Fiber Diet (After Healing)
Once you have fully recovered from a flare-up and your doctor gives you the green light, it is crucial to slowly reintroduce fiber into your diet. A high-fiber diet is the cornerstone of preventing future diverticulitis attacks. Fiber helps soften stool and add bulk, making it easier to pass. This reduces the pressure inside the colon and may help prevent new diverticula from forming.
Good sources of fiber include:
- Fruits: Apples, pears, berries, and oranges.
- Vegetables: Broccoli, carrots, Brussels sprouts, and squash.
- Legumes: Beans, lentils, and peas.
- Whole Grains: Oatmeal, brown rice, quinoa, and whole-wheat bread.
It’s important to increase your fiber intake gradually to allow your digestive system to adjust. Adding too much fiber too quickly can cause gas, bloating, and discomfort.
Other Lifestyle Changes for Prevention
Beyond diet, other lifestyle habits can contribute to better digestive health and help prevent diverticulitis flare-ups.
- Stay Hydrated: Drink plenty of water throughout the day. Water works with fiber to keep your stool soft and easy to pass. Aim for at least 8 glasses (64 ounces) of water daily unless your doctor advises otherwise.
- Exercise Regularly: Physical activity helps promote normal bowel function and can reduce pressure in the colon. Aim for at least 30 minutes of moderate exercise, like brisk walking, most days of the week.
- Maintain a Healthy Weight: Obesity is a known risk factor for diverticulitis. Losing excess weight can help lower your risk of developing complications.
- Quit Smoking: Smoking is linked to an increased risk of diverticulitis and its complications. Quitting can improve your overall digestive health.
By adopting these healthy habits, you can play an active role in managing your condition and minimizing the chance of future problems.
Frequently Asked Questions (FAQ)
Q1: Can stress cause my poop to look different with diverticulitis?
A: Stress doesn’t directly cause diverticulitis, but it can certainly affect your digestive system. Stress can trigger muscle spasms in the colon and alter bowel habits, leading to either diarrhea or constipation. For someone with diverticulosis, these stress-induced changes could potentially irritate the diverticula and contribute to a flare-up, thereby affecting what your poop looks like.
Q2: What should I do if I see blood in my stool?
A: If you see any amount of blood in your stool, you should contact your doctor right away. While it can be a symptom of diverticulitis, it can also be a sign of other serious conditions like colorectal cancer, ulcers, or inflammatory bowel disease (IBD). It’s crucial to get a professional medical evaluation to determine the cause and get the right treatment.
Q3: Are there foods I should always avoid if I have diverticulosis?
A: In the past, doctors used to advise people with diverticulosis to avoid nuts, seeds, and popcorn, fearing these small particles could get lodged in the diverticula and cause a flare-up. However, recent research has found no evidence to support this. For most people, a high-fiber diet that includes these foods is beneficial. The best approach is to listen to your body and discuss any concerns with your healthcare provider.
Q4: How long does it take for poop to return to normal after a diverticulitis flare-up?
A: The time it takes for your bowel movements to normalize can vary. It depends on the severity of the flare-up and how quickly you heal. As you slowly transition from a liquid/low-fiber diet back to a regular, high-fiber diet, your stools should gradually become more formed and regular. This process can take several days to a few weeks. Patience and a gradual dietary transition are key.
Q5: Is it possible to have diverticulitis without any changes in my stool?
A: While changes in bowel habits are a very common symptom, it is possible to have diverticulitis with other primary symptoms. Some people might experience intense, localized abdominal pain, fever, and nausea with minimal or no noticeable change in their stool. Everyone’s body responds to inflammation differently.
Conclusion
Navigating the symptoms of diverticulitis can be challenging, but understanding the potential changes in your bowel movements is a powerful first step. When considering what does poop look like with diverticulitis, remember that variations in shape, consistency, and color are often direct results of the inflammation and your body’s response to it. From thin, pellet-like stools to diarrhea and the presence of blood or mucus, these signs are your body’s way of telling you something is wrong.
While observing these changes is important for self-monitoring, it’s vital to rely on a healthcare professional for an accurate diagnosis and treatment. Prompt medical attention can help you manage a flare-up effectively and prevent serious complications. After recovery, embracing a high-fiber diet, staying hydrated, and leading an active lifestyle are your best defenses against future episodes. By partnering with your doctor and taking proactive steps, you can manage diverticulosis and maintain your digestive health for years to come.